How does the nose affect your sleep?
- Raymond
- May 16, 2019
- 3 min read
Updated: Sep 21, 2022
The function of the nose
The nose is an integral part of our respiratory system. We breathe all the time, usually through the nose. The nose functions to condition each breath so that the inhaled air is ‘ready’ for the lungs. It warms and humidify the air, and filter dust and any other environmental pathogens or irritants.
How does a blocked nose cause sleep apnoea?
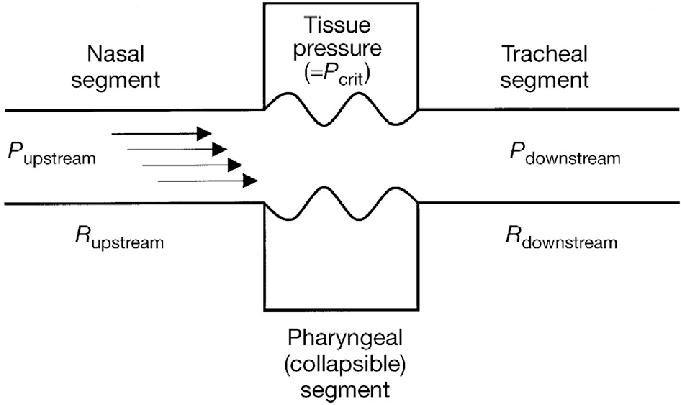
Humans are born obligatory nose breathers. If the nose is obstructed, breathing will be difficult. Recall those nights when you sleep with a stuffy nose e.g. when having the flu. Sleep becomes disrupted. You probably have woken up with headaches, facial congestion, dry throat, and an unrested sleep. This is because when our nose passage is obstructed, inspiration will be limited. There will be an increased respiratory effort. This not only leads to turbulent airflow but also further narrowing of the upper airway downstream due to Starling’s Law (see diagram below). The collapsed is maximum at the level of the pharynx. Our soft palate falls back against the back of the throat, shutting the throat from the nose. Alternatively, the palate flutters like a sheet of paper in the air. These lead to loud snoring and gasping. The tongue and pharyngeal wall collapsed inwards to further obstruct the airway. This phenomenon is what happens during obstructed sleep apnoea.
What is the natural way to overcome a blocked nose? Yes, we opened our mouth! This bypasses the nose and we can breathe again. However, mouth opening during sleep especially when sleeping on our back (supine), worsens the obstruction? Mouth opening causes the tongue to fall further backward and narrows the airway. This is worse when the person is overweight with a thick neck.
How do we know we are mouth breathing?

Mouth breathing during sleep can be subtle. Mouth opening dries the oral cavity and throat. It is more apparent if the aircon or the fan is blowing at the face. Hence, if you frequently wake up with the dry mouth or sore throat, you are probably mouth breathing.
Sleep apnoea and its assessment
Sleep apnoea is a phenomenon when there is the cessation of airflow during sleep. It can be obstructive, central, or mixed (both obstructive & central). Obstructive sleep apnoea accounts for the majority of cases especially among those who are obese. Obstructive sleep apnoea is due to obstruction of the upper airway during sleep due to loss of muscle tone during sleep. This leads to the collapse of the throat muscles and tongue and blocks the airway. Other causes of obstruction include swollen tissue within the nose, deviated nasal septum, large adenoids or tonsils. Thick subcutaneous fat around the neck also contributes to the amount of collapse and hence obstruction.
The sleep study is performed to determine the apnoea-hypopnoea index (AHI) which indicates the frequency of cessation of breathing or ineffective breathing leading to a dip in body oxygen. A nasendoscopy is performed to assess the anatomy of the upper airway, particularly to look for the causes of obstruction mentioned above.
Treatment of obstructive sleep apnoea
Treatment is a multi-modality approach. Weight loss is the most effective if the person is overweight. Positive airway pressure (PAP) overcome all levels of obstruction. The patient wears a mask connected to a pump which delivers positive pressure. This is an effective method of treating obstructive sleep apnoea. Compliance is sometimes an issue if there is high resistance from narrow nasal passages.
Treating the nose treats sleep apnoea.

Surgeries such as septoplasty (correct nasal septal deviation) and rhinoplasty (turbinate reduction) improve the nasal passage, reduce the pressure needed, hence improve PAP compliance. Relieving the nasal obstruction also corrects mouth breathing, reduces snoring, and improves pharyngeal (throat) obstruction. A clear nasal passage also reduced respiratory effort and hence negate Starling’s Law and reduces the collapsibility of the upper airway. An ear nose throat (ENT) doctor will be able to perform a full assessment of the airway and recommend the best treatment approach.
Dr. Lim Keng Hua is a graduate of the faculty of Medicine, National University of Singapore. He is a member of the Royal College of Surgeons in Edinburgh and a Master of Medicine in Otorhinolaryngology. He is an accredited specialist in otorhinolaryngology from the Ministry of Health (MOH) and Singapore Medical Council (SMC).
Dr. Lim Keng Hua was the first surgeon to be awarded a Clinical Rhinology Fellowship to Europe.
Dr. Lim has a whole realm of clinical experience, accumulated over more than 18 years of clinical practice. His special interest is in the diseases and allergies of the nose and sinuses. However, he is also well versed in the management of both adult and pediatric general ENT conditions such as ear infections, hearing loss, voice disorders, snoring & sleep disorders, salivary gland & thyroid swellings.
Ear Nose Throat, Head & Neck Surgery
+65 6735 9688
3 Mount Elizabeth, #03-01/02, Mount Elizabeth Medical Centre
Singapore 228510


Comments